
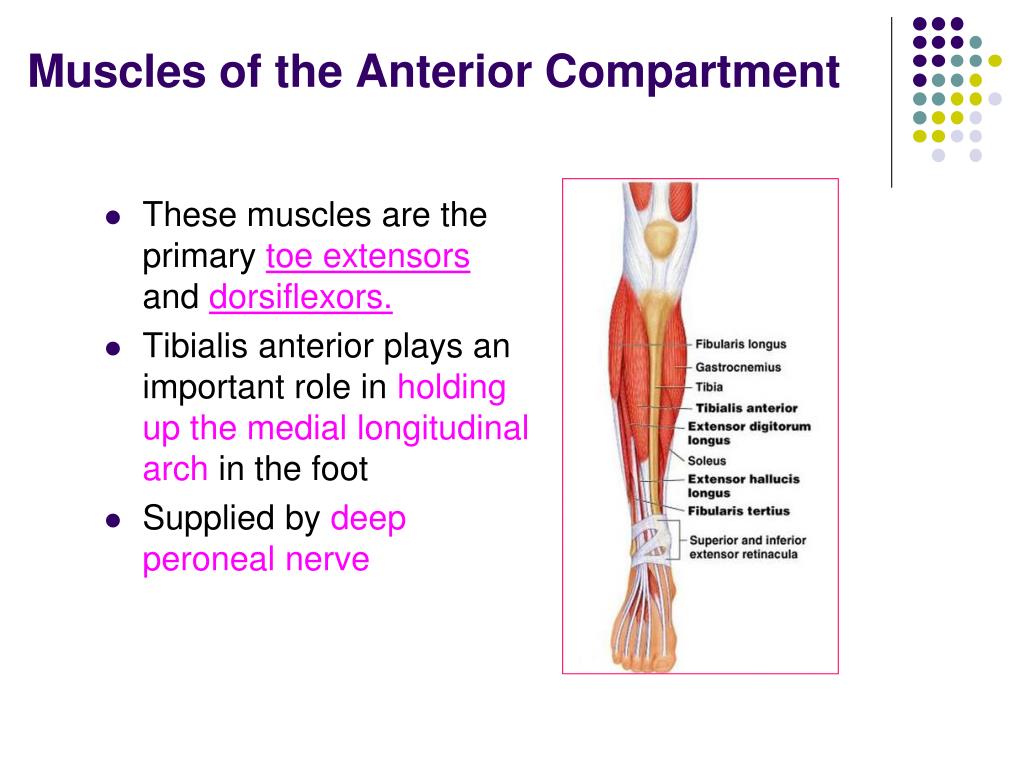
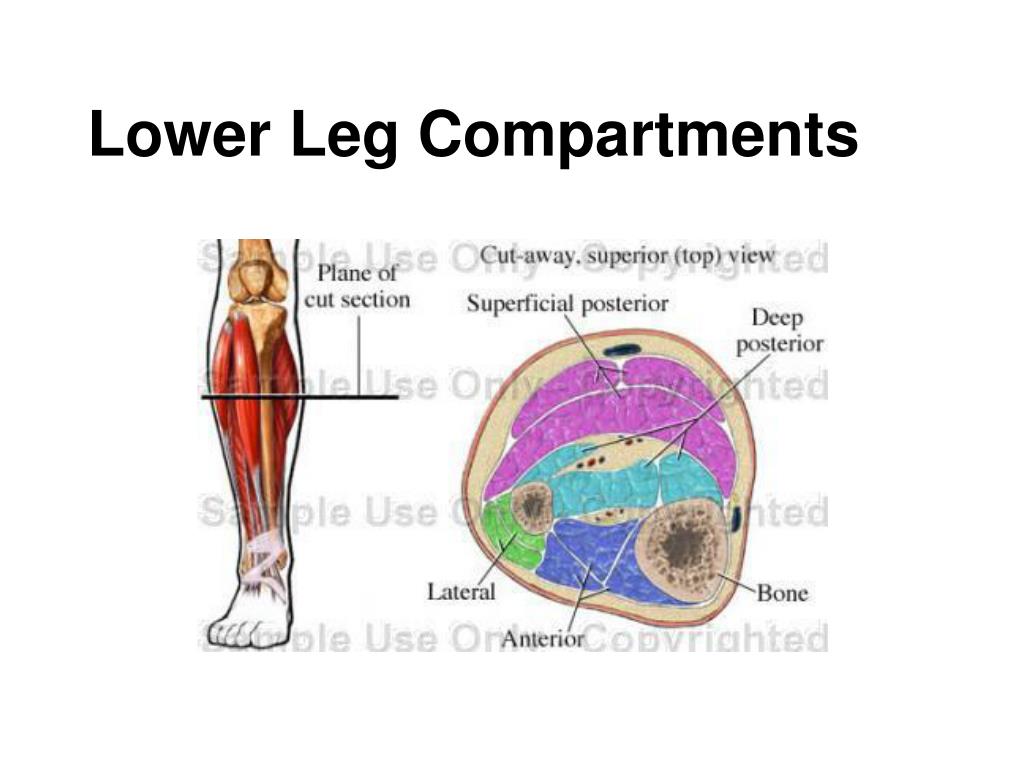
Patients evaluated directly after exertion may demonstrate edema and neurologic dysfunction on physical exam ( 5,6,9,27,31,37). It is important that only patients with historical clues suggestive of CECS have compartment testing performed. Currently there are no universally accepted diagnostic criteria for pathologic ICP values ( 1,29). If the history is not entirely convincing for CECS, it may be worthwhile to have the patient perform the exercise/exercise challenge that typically provokes the patient’s symptoms to determine whether their pain is consistent with CECS ( 14). This avoids unnecessary testing and, more importantly, subsequent referral for and even execution of surgical treatment ( 18,33). The lower leg contains four separate compartments, each bound by fascia and containing nerves and/or arteries and veins. Understanding the anatomy of the lower leg aids in localizing which compartment is affected based on the history and also guides catheter placement when measuring ICP (Fig. Figure 1:Ĭross-sectional anatomy of the left lower extremity compartments. The anterior compartment contains the tibialis anterior, extensor hallucis longus, and the extensor digitorum longus muscles. The compartment is bound medially by the tibia, posteriorly by the interosseous membrane, and laterally by the fibularis (peroneus) muscles. At the posterior medial border of the compartment lie the deep fibular (peroneal) nerve and the anterior tibial artery and veins. Symptomatic involvement may present as a mild foot drop, weakness with dorsiflexion, or paresthesias over the dorsum of the foot with the exception of the webspace between the first and the second digit and the far lateral aspect of the foot. The lateral compartment contains the fibularis (peroneus) longus and brevis muscles. It is bound anteriorly by the extensor digitorum longus muscle, medially by the fibula, and posteriorly by the edges of the flexor hallucis longus and soleus muscles. This can help reduce the size of the defect to be covered.Within this compartment lies the superficial fibular (peroneal) nerve at the anterior apex.
FASCIAL COMPARTMENTS OF LEG SKIN
Careful use of elastic retention sutures (elastic vessel loop woven through skin staples) can help counteract skin contraction, and be tightened progressively as swelling resolves. This is only permissible if it can be achieved without any skin tension it is inadvisable in smokers, who have impaired capacity for soft-tissue healing.įasciotomy wound edges tend to retract and become difficult to close. It is tempting to the surgeon to try early secondary skin suture, rather than skin-graft coverage, once the swelling has subsided. The simplest and safest technique is to cover the healthy soft-tissue defect with a split skin graft: at a later date, when the limb contours have returned to normal, the grafted area can be excised and secondary skin closure performed without tension. Once any skeletal injury is under control, the fasciotomy wound(s) healthy and the swelling of the soft tissues has sufficiently regressed, consideration must be given to achieving skin coverage. Reperfusion injury is another cause of compartment syndrome. After blood flow is restored, capillaries leak and ischemic muscle swells. An arterial injury may cause compartmental tissue ischemia.Muscle tolerates short periods of hypoxia, but after a few hours, progressive necrosis begins.
(MPP has also been called "Delta P", to indicate the difference between diastolic blood pressure and intramuscular pressure.) This difference in pressure reflects tissue perfusion far more reliably than the absolute intramuscular pressure.


 0 kommentar(er)
0 kommentar(er)
